Dr. Rajiv Nathoo performed five or six biopsies on a 54-year-old landscaper who presented to an Orlando dermatology clinic with a splotchy, painful rash. The rash was spreading from the man’s appendages to his face, yet past specialists had been befuddled by the thing was causing it.
The biopsy results affirmed Nathoo’s hunch, a conclusion he portrayed as something “you read in your course books”: leprosy.
Notwithstanding, the man didn’t have the undeniable gamble factors that most specialists would expect with the hard-to-get disease. Nathoo, a dermatologist and complex clinic director at Advanced Dermatology and Cosmetic Surgery Clinics in Orlando, began to believe that Central Florida might be an unexpected leprosy hotbed after observing a cluster of additional cases in the area.
Presently, his group is alerted other medical care suppliers to be watching out for comparative cases nearby.
Concurring an examination letter distributed by Nathoo and his partners in the diary Arising Irresistible Sicknesses, Focal Florida has revealed among the most noteworthy paces of uncleanliness in the US.
The World Health Organization estimates that 159 cases will be reported nationwide in 2020, compared to 200,000 new cases each year worldwide. The new letter says Focal Florida represented 81% of cases in Florida and almost 1 out of 5 uncleanliness cases from one side of the country to the other.
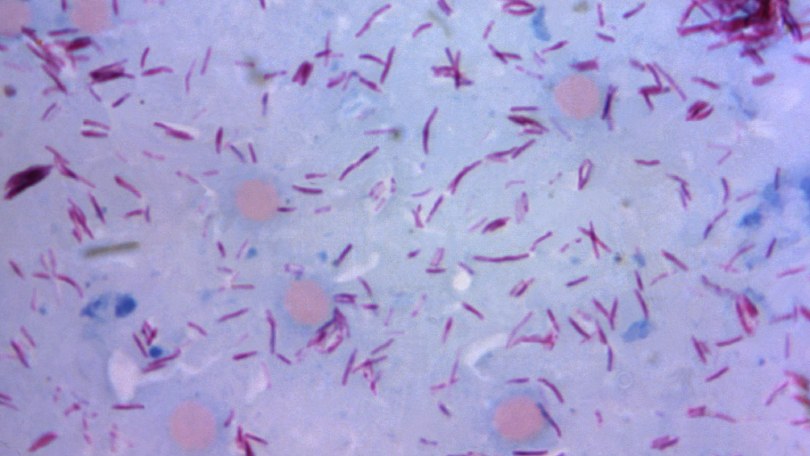
Otherwise called Hansen’s infection, sickness is brought about by the microbes Mycobacterium leprae, which assaults nerves under the skin. Researchers aren’t totally certain of how it spreads, yet most accept that it’s sent through drops when a contaminated individual hacks and wheezes. Lesions and rashes that are numb or devoid of sensation due to nerve involvement are its distinctive symptoms.
Nine-joined armadillos in the Southeastern US can likewise convey the microbes, and quality examinations have connected human diseases to the sickness strains conveyed by armadillos, in spite of the fact that it’s not generally clear the way in which people experience armadillo-conveyed microscopic organisms. Numerous patients can’t remember truly having contact with the creatures.
The sickness isn’t communicated through relaxed contact like shaking hands or sitting close to a contaminated individual. According to the US Centers for Disease Control and Prevention, spreading leprosy necessitates prolonged close contact with an untreated person for many months. Generally 95% of individuals aren’t defenseless to the disease on the grounds that their insusceptible frameworks are hereditarily customized to oppose it.
Subsequently, sickness is an uncommon illness in the US. By and large, most instances of uncleanliness in the US influence individuals who travel to nations with high paces of illness or who are presented to armadillos that convey the sickness.
However, there are instances in which doctors are unaware of the individual’s exposure.
“In specific states, we see a larger number of cases than others. Florida is one of them, according to Dr. Linda Adams, chief of the laboratory research branch at the National Hansen’s Disease Program, a federal program that coordinates treatment for Americans diagnosed with the condition. Around there, we truly do see cases that we can’t make sense of. There’s been no unfamiliar travel, for instance, or no contact with armadillos.”
Even though he spent a lot of time outside, the 54-year-old man in the new report told his doctors that he had never left the state of Florida, had never met armadillos, or had long-term interactions with people from countries with high leprosy rates.
Around 34% of new cases somewhere in the range of 2015 and 2020 didn’t have those conventional gamble factors, as per the examination letter. All things considered, individuals seem to have been contaminated locally, a finding that recommends that disease has become endemic in Florida, the letter says.
Experts concur that the region is experiencing an epidemic of leprosy. However, that need not cause a general wellbeing alarm, said Dr. Nicole Iovine, boss medical clinic disease transmission specialist at the College of Florida Wellbeing Shands Emergency clinic. ” Endemic” basically implies there are customary levels of a sickness in a locale however not that rates are climbing, she made sense of.
“It’s truly interesting still,” Nathoo said. ” Here, these numbers are still extremely low. We’re not that worried about it.”
However, over the course of the past five years, Nathoo has located the clinical records of 15 cases of leprosy with biopsy evidence that have been clustered in eastern Orlando and Volusia County. Fourteen of them have not gone external the US, and not a solitary one of them is associated with one another in any capacity.
According to Dr. Charles Dunn, a study author and chief resident at Advanced Dermatology and Cosmetic Surgery Clinics, there is a misconception among physicians that leprosy only affects foreign-born individuals or those who have been exposed to nine-banded armadillos, despite the fact that there is a “strong geographic predilection” for the disease in central Florida.
Since their patients coming up short on conventional gamble factors, Dunn trusts that it merits dispersing those suspicions. Despite the fact that armadillos are the “typical case,” there is no ideal vector for uncleanliness that the clinical local area can pinpoint, he added. All things considered, the vast majority don’t have delayed contact with nine-grouped armadillos.
“That was the essence of our paper, to say, ‘hello, this person strolled into our center. We’ve analyzed him, and when we take a gander at our data set of individuals in Florida, they appear to be collected here,’ ” Nathoo said. ” You should just keep an eye out for that.”
Iovine is still concerned about the cluster of potentially endemic cases in Central Florida. Left untreated, the illness can incapacitate the hands and the feet, cause visual impairment, and prompt fingers and toes to abbreviate. The infection can be treated, but it needs to be treated over several years with a combination of antibiotics.
Additionally, a cure may not be able to repair nerve or skin damage in patients whose diagnosis has been postponed, which is a common occurrence in the United States, where physicians are unfamiliar with the disease.
One of the difficulties with sickness is the way leisurely the microscopic organisms develops. The CDC says that symptoms like pale, numb blotches, rashes, ulcers, and lesions can take up to 20 years to appear depending on the type of infection.
Considering that deferral, following the source and spread of an uncleanliness infection can challenge. Furthermore, since most specialists “won’t ever see an instance of disease,” Iovine said, it’s frequently misdiagnosed from the get go.
“I’m certain that patients go for a really long time without a right conclusion,” she said. ” I’d say that’s much more common.
In the new review’s case report, the patient had clinical indications of uncleanliness for a considerable length of time prior to coming to Nathoo and being evaluated for Hansen’s sickness. Prior to that, numerous providers had indicated that they lacked an understanding of his condition.
The National Hansen’s Disease Program sends specialized antibiotics to the provider’s office and begins a contact-tracing process once the provider has reported leprosy to the state health department within 24 hours.
“The side effects of sickness are many times missed, as it’s only not on the dermatologist’s radar,” Adams said. ” It’s not the principal thing they consider when they see something like this.”